Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (219 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

b. Secondary hypogonadism. It accounts for approximately 2% gynecomastia cases. It is usually due to a hypothalamic or pituitary abnormality. Pituitary abnormality includes infarction and adenoma. Men with hyperprolactinemia show erectile dysfunction and loss of libido but can also develop galactorrhea and gynecomastia. Prolactin levels >200 ng/mL are almost always indicative of a pituitary tumor. The principal mechanism is through prolactin’s indirect effects on reducing the secretion of gonadotropins, thereby resulting in a shift in the estrogen–testosterone balance favoring estrogen.
6. Testicular neoplasms. The mechanism is related to elevation of the estrogen level either by direct production from the tumor cells or through stimulation of interstitial cells by beta-HCG. Approximately 20% of Leydig cell tumors and 33% of Sertoli cell tumors are associated with gynecomastia. These non–germ cell tumors cause gynecomastia through increased production of estrogen by the tumor cells. Germ cell tumors, on the other hand, under the influence of beta-human chorionic gonadotropin (HCG), cause a disproportionate increase in the production of estrogen over testosterone.
7. Hyperthyroidism. Gynecomastia has been reported in 10–40% of men with Graves disease.
8. Chronic renal failure. Gynecomastia occurs in approximately 50% of patients treated with maintenance hemodialysis. The mechanism of gynecomastia in renal failure is multifactorial.
a. Renal failure is associated with an increased luteinizing hormone (LH) level, which stimulates the production of estradiol by the Leydig cells.
b. Other etiologies include low testosterone levels related to primary testicular dysfunction and hyperprolactinemia related to deceased clearance.
c. Increased prolactin levels, linked to secondary hyperthyroidism, may also contribute.
9. Other rare causes include feminizing adrenocortical tumors, ectopic HCG production by tumors of the lung, liver, and gastrointestinal tract, true hermaphroditism, androgen insensitivity syndromes, and aromatase excess syndrome.
Who Should Be Suspected?
Combination of a careful history and physical examination and a few diagnostic tests can result in the identification of the cause of gynecomastia in the majority of patients.
I. History:
A. Pain. Gynecomastia tends to present with discomfort, as opposed to breast cancer, which is more typically painless.
B. Symmetry. Gynecomastia is often bilateral, albeit asymmetrically, whereas breast cancer is often unilateral.
C. Medication history
D. Assess for other historical features of family history of cancer, rapid onset, older age, and breast discharge (which suggests breast cancer).
E. Assess for loss of libido and erectile dysfunction (which suggests hypogonadism).
F. Check for a history of liver disease or for risk factors associated with liver disease, chronic renal insufficiency, a pituitary mass, thyroid dysfunction, or Cushing syndrome.
G. Check for symptoms of an underlying malignancy, specifically focusing on testicular, lung, and gastrointestinal sources.
H. Assess weight changes and refeeding.
II. Physical examination:
1. Breast examination.
a. Breast cancer usually manifests as a hard nodule that is fixed to the underlying soft tissue. Other characteristics include a unilateral presence, nipple discharge, eccentric positioning, skin ulceration, and axillary adenopathy.
b. Gynecomastia is usually characterized by firm, rubbery, well-defined masses, discoid in shape, mobile, concentric with origination beneath the nipple or areolar region, frequently bilateral, and tender to palpation. Unilateral gynecomastia may be seen as a stage in the development of bilateral gynecomastia. Asymmetry is a frequent finding in patients with gynecomastia.
2. Testicular examination. Assess for signs of hypogonadism or neoplasm.
3. Neurologic examination. Assess the visual fields and cranial nerves.
4. Palpate the thyroid gland for size and nodularity.
5. Assess for stigmata of Cushing syndrome (strength, striae, fat pad distribution, hirsutism).
Laboratory Findings (Figure
6-9
)
1. Initial evaluation should include:
A. Beta-HCG level, obtained for the evaluation of ectopic production.
B. Serum total and free testosterone, LH, follicle-stimulating hormone (FSH), and estradiol concentrations.
C. Chest radiograph can be used to rule out pulmonary malignancy.
2. Supplemental hormonal evaluation is performed as determined by clinical judgment.
A. Prolactin levels should be obtained in any patients with suspicion of a mass lesion or erectile dysfunction, or when secondary hypogonadism is identified (i.e., low testosterone or low to normal LH).
B. Dehydroepiandrosterone sulfate (DHEAS) assesses for adrenocortical tumor in the setting of elevated estradiol.
C. TSH and overnight dexamethasone suppression test (or 24-hour urinary free cortisol).
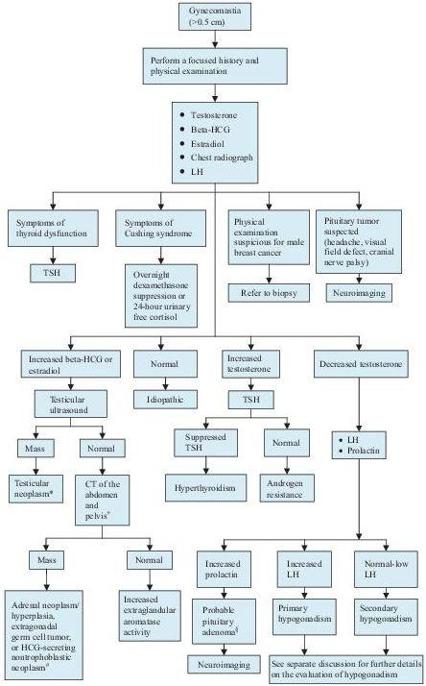
Figure 6–9
Algorithm for the workup of gynecomastia. CT, computed tomography; HCG, human chorionic gonadotropin; LH, luteinizing hormone; TSH, thyroid-stimulating hormone. *The neoplasm is likely a germ cell tumor if the HCG is elevated, or a non–germ cell tumor if the estradiol is elevated.
+
Abdomen and pelvic images are obtained to identify either an extragonadal germ cell tumor or an HCG-secreting nontrophoblastic neoplasm. An adrenal mass or hyperplasia is sought if the estradiol is elevated.
#
Common nontrophoblastic neoplasms include lung and gastrointestinal sources.
§
An elevated prolactin level may be seen secondary to hypothyroidism, resulting from an elevated TSH. A number of medications can elevate the prolactin level. Before proceeding with neuroimaging, be certain to exclude these possibilities. A prolactin level
>
200 ng/mL is usually indicative of an adenoma.
Imaging Studies (see Figure
6-9
)
Neuroimaging should be reserved for those cases in which a mass lesion is suspected (e.g., headache, visual field defect, cranial nerve palsy) or the hormonal evaluation leads one to suspect a pituitary tumor (i.e., elevated prolactin level or Cushing disease).
Suggested Readings
Braunstein GD. Causes and evaluation of gynecomastia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Braunstein GD. Epidemiology and pathogenesis of gynecomastia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
HIRSUTISM
Definition
Hirsutism refers to the presence of excess terminal hair in androgen-dependent areas in women, including face, chest, areola, linea alba, lower back, buttock, inner thigh, and external genitalia.
Overview