Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (522 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
12.87Mb size Format: txt, pdf, ePub
TABLE 12–1. Staging of Acute Kidney Injury
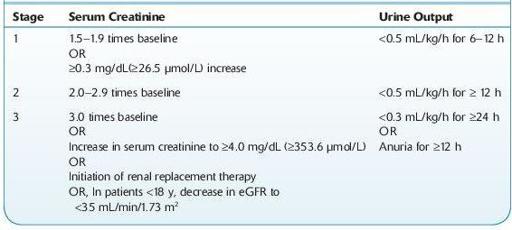
eGFR, estimated glomerular filtration rate.
Source: Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group.
KDIGO clinical practice guideline for acute kidney injury.
Kidney Int.
2012;2(Suppl):1–138.
Who Should Be Suspected?
Patients with AKI present in a variety of ways:
Patients with symptoms suggestive of uremia. The term uremia describes the clinical syndrome associated with retention of the end products of nitrogen metabolism due to severe reduction in renal function. It can be a consequence of either acute or chronic renal disease.
Patients with oliguria (urine output of <500 mL/day) or anuria (urine output <100 mL/day).
Patients with an elevated serum creatinine level.
Hospitalized patients with severe losses of extracellular fluid or patients exposed to nephrotoxic drugs, sepsis, or radiographic contrast agents who demonstrate the symptoms or findings described above.
Laboratory Findings
Urinalysis is the most important noninvasive test in the diagnosis of AKI and its etiology (see Figure
12-1
). Microscopic examination is normal in most cases of prerenal disease. The presence of RBC casts or dysmorphic RBCs indicates glomerular disease, whereas finding cellular debris or granular casts suggests ischemic or nephrotoxic AKI. Urine specific gravity is of limited value in establishing the etiology of AKI.
Glomerular filtration rate (GFR) gives an approximate estimation of the number of functioning nephrons and may be markedly reduced in patients with AKI. Estimation of GFR has a prognostic rather than diagnostic utility in AKI.
Serum creatinine level is elevated at diagnosis and continues to rise. The rate of rise may be helpful in determining the etiology of AKI.
Blood urea nitrogen (BUN)/serum creatinine ratio is normal in intrinsic renal disease (10–15:1) and elevated (>20:1) in prerenal azotemia.
Urine-to-serum creatinine ratio is high in patients with prerenal disease and low with renal causes of AKI.
Other books
Women's Bodies, Women's Wisdom by Christiane Northrup
Bound to the Alpha: The Bundle by Viola Rivard
Bayou Trackdown by Jon Sharpe
Splitting Up and Park Hyatt Hotel by Galatée de Chaussy
Pure Lust Vol. 2 by Parker, M. S., Wild, Cassie
The Art of Keeping Secrets by Patti Callahan Henry
Total Rush by Deirdre Martin
Entangled With the Thief by Kate Rudolph
The Second-last Woman in England by Maggie Joel
Ascending by James Alan Gardner