Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (642 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Another less common immunologic cause for platelet refractoriness is antibodies to antigens present on platelets other than HLA. Patients with these plateletspecific antibodies will require platelet products from rare donors that lack these antigens. The most commonly encountered antibody to a platelet-specific antigen is anti–HPA-1a (anti-Pl
A1
).
In addition to these immunologic causes, there are many nonimmune causes for an inadequate response to platelet transfusion. These include fever, sepsis, disseminated intravascular coagulation (DIC), splenomegaly, bleeding, as well as treatment with certain medications. Most of these reasons for refractoriness may persist until the patient’s underlying medical condition is adequately treated.
GRANULOCYTE TRANSFUSION
Granulocyte transfusion has decreased dramatically over the last two decades. Previously, granulocytes were frequently transfused to neutropenic patients undergoing chemotherapy or to patients with congenital neutrophil abnormalities (e.g., chronic granulomatous disease) who had infections.
Who Should Be Suspected?
Due to advances in antimicrobial therapy, granulocytes are now only transfused to patients who are temporarily neutropenic and have a life-threatening bacterial or fungal infection that is unresponsive to antimicrobial therapy. Based on published literature, it is not clear if the addition of granulocyte transfusion provides any benefit when compared to antimicrobial therapy alone. The published studies have had variable conclusions, but there appears to be a trend toward benefit in the studies that have transfused higher doses of granulocytes with each transfusion. If a decision is made to transfuse granulocytes, generally one product is transfused daily until the patient has an absolute neutrophil count above 500/μL.
Granulocytes are collected using an apheresis device from healthy volunteer donors. However, granulocyte transfusion carries significant risks. Some of the risks include CMV transmission, HLA immunization, and severe pulmonary reactions. Additionally, granulocytes must be transfused the same day that they are collected and thus are transfused prior to the completion of standard infectious disease testing performed on blood donors. Platelet donors who recently had negative infectious disease testing are often used as granulocyte donors, but there remains a risk of infectious disease transmission. As with any other blood product transfusion, the risk– benefit ratio must be carefully examined prior to the transfusion of granulocytes.
RISKS AND ADVERSE CONSEQUENCES RELATED TO BLOOD PRODUCT TRANSFUSION
Transfusion of blood products may be life saving but also carries a significant risk of adverse consequences for the recipient (Table
15-4
). Some of the possible adverse consequences that have been well documented include infectious disease transmission, transfusion-associated immunomodulation, and transfusion reactions.
TABLE 15–4. Adverse Effects of Blood Transfusions
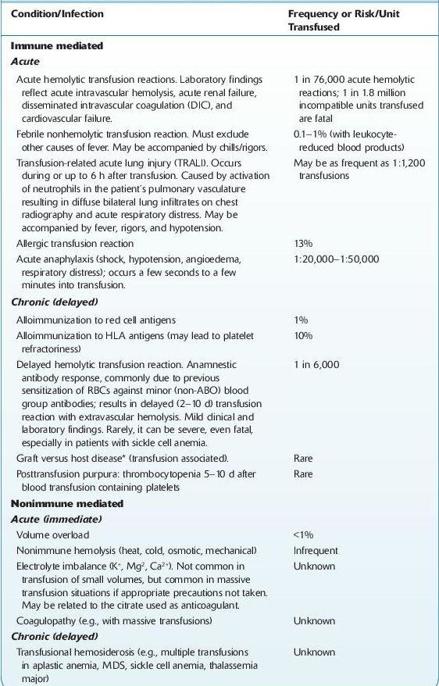
*
Transfusion-associated graft versus host disease (TA-GVHD)
occurs when immunocompetent T lymphocytes are transfused into a patient who cannot reject them, and they engraft in the recipient, proliferate, and mount an immune attack against the host tissues. TA-GVHD occurs 4–30 d after transfusion of any cellular blood component. It may occur in a nonimmunocompetent recipient or in an immunocompetent recipient who receives histocompatible donor lymphocytes, especially from blood relatives, which can recognize a different HLA haplotype in the recipient. There are molecular techniques to diagnosis TA-GVHD. Mortality is nearly 90% in the full-blown syndrome. Irradiation of blood products virtually eliminates the risk of this complication. †Estimates published by the British Committee for Standards in Haematology.
Considerations
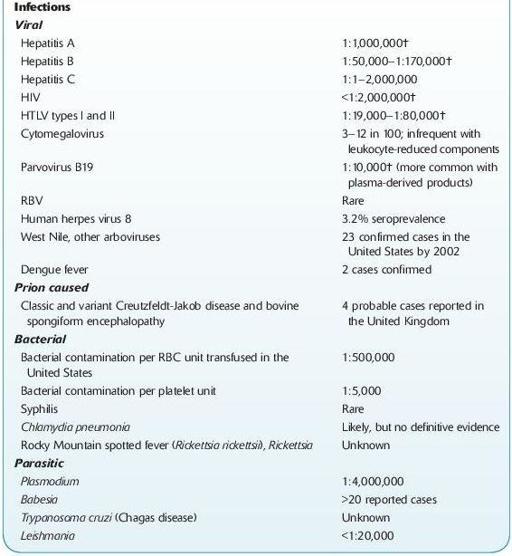
Transfusion of blood products has resulted in transmission of bacteria, viruses, parasites, and prions. In order to minimize the risk of transmission of these infectious agents, donors are screened using a donor history questionnaire. Subsequently, each donor is tested for several transmissible infectious diseases with each donation. If any of the infectious disease testing is positive, the blood product is discarded and the donor is deferred from subsequent donation as appropriate. The donor screening process and infectious disease testing have significantly decreased the risk of infectious disease transmission over the last three decades.
Other possible adverse consequences of blood product transfusion include transfusion reactions (TR). The most common transfusion reactions include allergic transfusion reactions (ATR) and febrile nonhemolytic transfusion reactions (FNHTR), while hemolytic transfusion reactions (HTR), transfusion-related acute lung injury (TRALI), and transfusion-associated circulatory overload (TACO) are the leading causes of morbidity and mortality related to transfusion.
ALLERGIC TRANSFUSION REACTIONS
ATRs are usually caused by the transfusion of foreign plasma proteins. The majority of allergic reactions are limited to skin manifestations such as urticaria, erythema, and pruritus. These reactions can be treated with antihistamines and/or corticosteroids. If allergic reactions prove to be recurrent, the patient can also be premedicated with these medications. A minority of patients may have more severe ATRs that may involve the patient’s airway (e.g., laryngeal edema). On rare occasion, it is also possible that a patient may have an anaphylactic reaction, which presents with hemodynamic instability in addition to the symptoms seen in a severe allergic reaction. In these patients, beta-adrenergics and aggressive supportive care may be necessary.
Who Should Be Suspected?
Although the cause of anaphylactic transfusion reactions is often unknown, classically they have been described in IgA-deficient patients with anti-IgA antibodies shortly after initiation of a blood product transfusion. If additional transfusion is required in patients with a history of severe allergic or anaphylactic transfusion reactions, red cells and platelets should be washed to reduce their plasma content. Plasma should only be transfused in these patients if it is lifesaving and should be from IgA-deficient donors if the patient is IgA deficient.
FEBRILE NONHEMOLYTIC TRANSFUSION REACTIONS (FNHTR)
FNHTRs present as reactions where a rise of ≥1°C is seen, possibly with associated chills/rigors. These reactions are usually self-limited and may be mitigated by treatment with antipyretics. Prior to the reaction being declared an FNHTR, investigation to exclude other causes is imperative as fever may be a component of other types of transfusion reactions (such as HTRs).
HEMOLYTIC TRANSFUSION REACTIONS (HTR)
HTRs result from the transfusion of incompatible blood products. The most common cause of HTRs is transfusion of incompatible red cells. The alloantibody causing the HTR can be to ABO antigens or other blood group antigens. The incompatible transfusion may have been caused by an error in patient identification (during sample acquisition or blood product transfusion), an error when performing the type and screen (or crossmatch), or an error when issuing the blood product.
Who Should Be Suspected?