Whole (21 page)
Authors: T. Colin Campbell

I am convinced that our committee’s decision not to go down that path of estimating the size of such an unknowable risk was wise. Even today, writers incorrectly claim with far too much assurance that one-third of all cancers are preventable by dietary means, based on that University of Oxford report. Precise numbers are often over-interpreted, especially by those with a personal or professional agenda. And decades later, diet and health research communities still cannot agree on a precise figure.
The problem is, risk doesn’t actually exist as an objective reality. It changes constantly based on how much we know. For example, the
television station that broadcast the Washington Nationals’ baseball games used to display a statistic they called “odds of winning.” If the Nationals were ahead 5-2 in the bottom of the fourth inning, their odds of winning that game might be 79 percent. But if the opposing team then scored a run in the top of the fifth inning, those odds might decline to 65 percent. A grand slam by the Nationals in the eighth inning would raise those odds again, perhaps to 97 percent. But a heroic rally in the top of the ninth could erase that lead and shift the odds yet again. The problem, of course, is that the odds of winning can’t be permanently pinned down. Every pitch, every swing of the bat, every change in cloud cover or drop in relative humidity could conceivably affect the final score. Depending on what the statistician who programmed the algorithm chose to include or ignore, the number could change dozens of times each second.
Like a bookmaker seeking precise quantification of risk to set odds on the outcome of a baseball game, individuals who care about their own health and that of their loved ones also seek the reassurance of specific percentages. They want to know with some confidence how to stay healthy and avoid chronic disease. But they don’t need misleadingly “accurate” aggregate numbers that predict nothing in any specific instance. The important takeaway from our report wasn’t how much cancer was preventable by diet, but that diet was a predominant factor.
What can we do, then, if we can assume neither a specific estimate nor a wide range of possible estimates? Do we just make up stuff? I am convinced that most people simply believe what they want to believe about cancer causation and prevention, according to which way the nature-nurture pendulum swings in their minds. In the absence of a reliable answer to the cancer prevention question, they fall back on personal nature or nurture biases.
Where we stand on this continuum, consciously or unconsciously, influences our thinking about health and disease more than we realize. Do we simply accept the cards dealt to us, or do we consider the possibility that we can control our own destiny? If our health trajectory is mostly
predetermined by our genes, then there’s no point in trying to be healthy. If our choices trump the cards we were dealt at birth, then there’s a reason for us to do what we can to achieve and maintain health.
Most medical researchers fall on the nature side of the nature-nurture dichotomy, and affirm the primacy of genetics as the basis of disease. They mistakenly believe that genetics is what will allow us to better diagnose and predict disease risk, through the discovery of faulty genes or gene arrangements in DNA that may be causing disease. Basic to these beliefs is a theory fairly popular in the health sciences called
genetic determinism.
According to this theory, we can draw a more or less straight causal line between genes and their final health- or disease-related outcomes. In other words, genes operate fairly independently, continuing to “do their thing” with little impact from the environment and one’s lifestyle. A very simple representation of this process is shown in
Figure 8-3
.
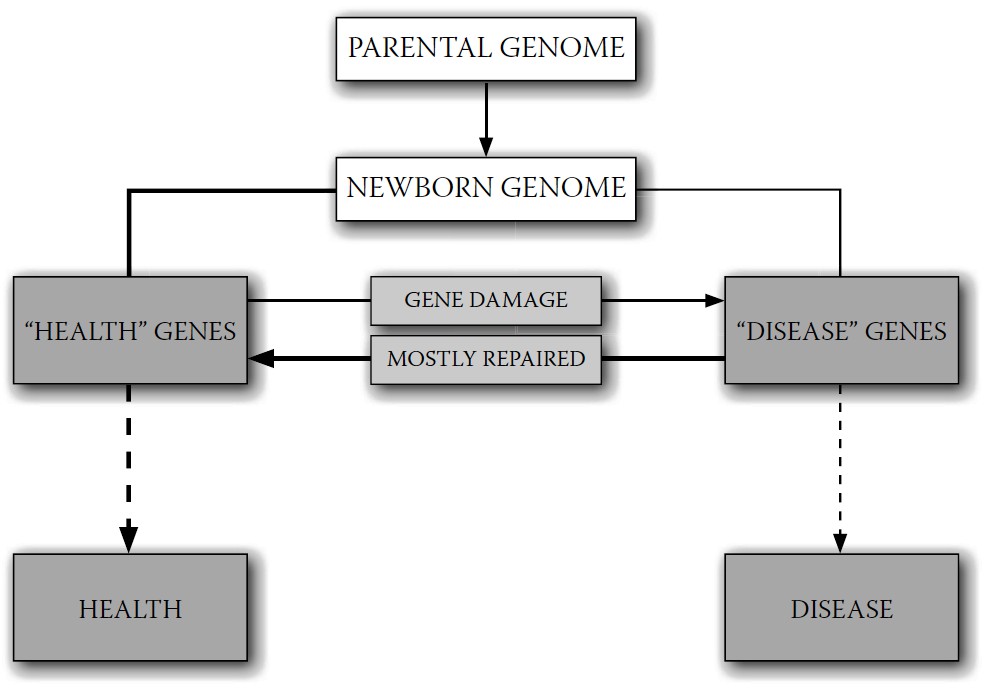
FIGURE 8-3.
Genetic determinism
Health or disease occurrence is primarily determined by “health” and “disease” genes, which arise from the newborn’s genome plus damaged but unrepaired genes produced during life.
In contrast, there is an alternative belief system to genetic determinism that I call
nutritional determinism,
wherein nutrition controls the
expression of genes to cause health or disease outcomes, by turning on health genes and suppressing disease genes as shown in
Figure 8-4
. And this is the belief system to which, based on my years of research and that of others, I subscribe.
Certainly, there also are nonnutrient lifestyle factors that may control gene expression. There are also, of course, relatively rare diseases like Tay-Sachs and others that are entirely genetic in cause, for which nutrition may, at very best, be able to mitigate some of their symptoms—if that. Even nutrition is not a cure-all; there’s no diet that can regrow an amputated limb, as far as we know. However, I am suggesting that nutritional inputs are the primary factor in gene expression, and that in the vast majority of cases, the vast majority of the time, good nutrition has a much greater impact than anything else—including the most complicated and expensive genetic intervention.
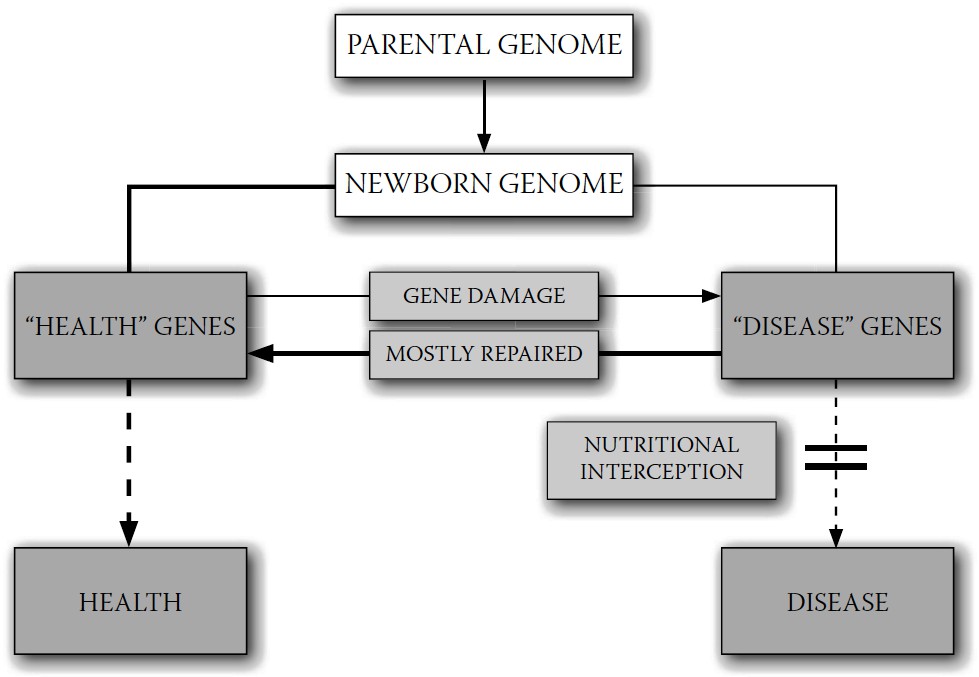
FIGURE 8-4.
Nutritional determinism
Health or disease processes begin with “health” and “disease” genes, but nutritional practices control expression of these genes. Good nutrition blocks expression of disease genes, leaving health genes to produce health.
Genes are the starting point for health and disease events; they are the “nature” part of the equation. But it is nutrition and other lifestyle
factors, the “nurture” part, that control whether and how these genes are expressed. The influence of nurture (i.e., nutrition) has far more influence on health and disease outcome than nature (i.e., genes).
A belief in genetic determinism suggests that our future health and disease events are already predestined at birth and that, as we age, we simply move from one disease benchmark to another according to the genetic blueprint we inherited at conception. This encourages the impression that there is little or nothing that we can do to prevent serious diseases like cancer. In contrast, the belief that cancer and related diseases are dependent on nutritional practices can encourage a sense of hope and lead to healthier behavior. And as we’re about to see, this belief is not just wishful thinking; it’s supported by an overwhelming amount of wholistic evidence. Let’s now look at how nutrition and genetics compare when it comes to minimizing and repairing our damaged and misbehaving genes, and what our focus on a reductionist approach to disease means for our ability to prevent chronic diseases like cancer.

The saddest aspect of life right now is that science gathers knowledge faster than society gathers wisdom.
—
ISAAC ASIMOV
W
e all get sick. Most of the time it’s no big deal. In the memorable words of physician and writer Lewis Thomas, “The great secret of doctors, known only to their wives, but still hidden from the public, is that most things get better by themselves; most things, in fact, are better in the morning.” Our bodies take care of any illness fairly quickly, no intervention needed (especially if we’re eating a WFPB diet). If not, we go to the doctor or, if it’s very serious, to a hospital. These are normal aspects of modern life that most of us take for granted. Yet most people don’t really understand disease and where it comes from: why we get sick and what role our DNA plays in letting or making that happen.
As we discussed briefly in
chapter eight
, genes are the starting point of both health and disease. They are the source for all our biological reactions that, in effect, lead to bodily form and function—what we call life. Some of our genes start reactions that lead to health. Others lead to disease.
The vast majority of our genes are the health-giving kind—otherwise, we wouldn’t last very long. These are the genes that form our cells, our organs, and our bones; that regrow skin after a cut or scrape; that make apples taste sweet and poisonous mountain buckthorn berries bitter. A small number of our genes, however, produce disease.
All disease starts with genes and gene combinations; what we call
diseases
are the end stages of interactions between our genes and elements from our environment, through the medium of our bodies. We get the flu, for example, because our genes produce certain symptoms in response to a particular microbe. We even bleed (and clot) when we get a paper cut because our genes have programmed that response into our physiologies. If our genes have made us hemophiliacs, it means that bleeding, once it’s started, is harder to stop. This interaction between genes and environment isn’t just the case for short-term illnesses like the flu or conditions like hemophilia. Our genes also trigger chronic diseases like cancer, heart disease, and diabetes in response to environmental stimuli (e.g., our diet, especially over a long period of time).
Our health-producing genes come from our parents. Where do our disease genes come from? There are two main sources. Some come from our parents and their ancestors before them; they are present in our initial germ or embryo. Other disease-causing genes may begin as health-giving genes that become damaged by mutation during our lifetimes.
These mutations are widely thought to be caused mostly by unnatural, synthetic chemicals that pollute our environment; we’ve already seen how oxidation reactions in our cells can produce such mutations. But these chemicals are not the only agents causing this kind of gene damage. Low levels of certain natural chemicals and other aspects of our environment (e.g., cosmic radiation, excessive sunlight, numerous chemicals in plants
and microorganisms) can do the same thing. Together, these natural and unnatural chemicals cause continual low-level genetic damage during our lifetimes.
The good news is, our bodies have learned how to routinely repair such damage. Our cells have a repair capability that works remarkably well right after the damage occurs. They had to have developed such a capability, or our evolutionary ancestors, subject to the same exposure to natural chemicals that we are today (and much less medical care), would not have survived long enough to reproduce. But this process of repair is not perfect. A very small percentage of the genes damaged during our lifetime are not repaired and may spawn successive generations of damaged cells as our tissues are renewed.
Perhaps surprisingly, this small percentage may not be all that bad. Some mutated genes turn out to be beneficial, and contribute to human evolution as their carriers survive and reproduce in greater numbers than the non-mutated population. Mutations are how evolution works. But while that low level of damage is useful for humanity as a whole, it can be less beneficial to individuals, because often these mutated genes are the source of disease.
The aim of health professionals who focus on chronic disease caused by this long-term damage is therefore two-fold: to prevent as much of that damage as possible, and to treat as many of the effects of that damage— what we call disease—as possible. And genetics, at least right now and probably indefinitely, is not a very good place to begin either of these efforts.