Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (610 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
3.94Mb size Format: txt, pdf, ePub
Respiratory alkalosis is associated with a pCO
2
<35 mm Hg.
Therefore, mixed metabolic and respiratory acidosis is characterized by low pH, low HCO
3
−
, and high pCO
2
.
Mixed metabolic and respiratory alkalosis is characterized by high pH, high HCO
3
−
, and low pCO
2
.
In severe metabolic acidosis, respiratory compensation is limited by inability to hyperventilate pCO
2
to less than approximately15 mm Hg; beyond that, small increments of the H
+
produce disastrous changes in pH and prognosis; therefore, patients with lung disorders (e.g., COPD, neuromuscular weakness) are very vulnerable because they cannot compensate by hyperventilation. In metabolic alkalosis, respiratory compensation is limited by CO
2
retention, which rarely causes pCO
2
>50–60 mm Hg (because increased CO
2
and hypoxemia stimulate respiration very strongly); consequently, pH is not returned to normal (Table
13-6
).

Base excess (BE)
BE hypothetically “corrects” pH to 7.40 by first “adjusting” pCO
2
to 40 mm Hg, thereby allowing comparison of resultant HCO
3
−
with normal value at that pH (24 mmol/L). Normal = −2 to +2 mmol/L.
BE can be calculated by determined values for pH and HCO
3
−
by this formula:
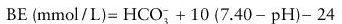
Negative BE indicates depletion of HCO
3
−
. It does not distinguish primary from compensatory derangement.
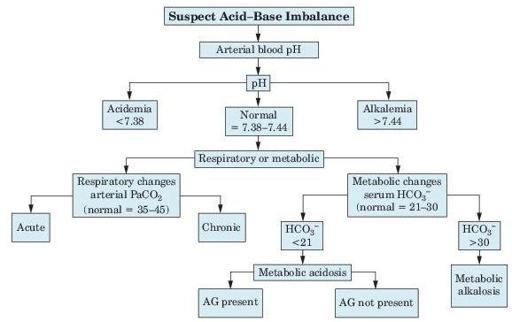
Figure 13–2
Algorithm for acid–base imbalance and anion gap (AG).
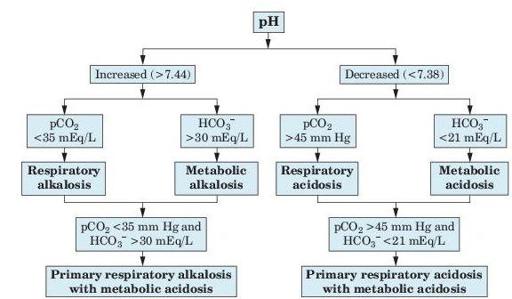
Figure 13–3
Algorithm illustrating effects of metabolic and respiratory acid–base changes in blood.
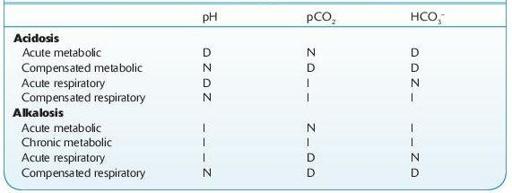
TABLE 13–2. Metabolic and Respiratory Acid–Base Changes in Blood
Other books
Nick's Blues by John Harvey
Eternal Echoes, Emblem of Eternity Trilogy Book 2 by Angela Corbett
Promised to the Crusader by Anne Herries
Lure by Rathbone, Brian
Topping the Domme (Crime and Punishment) by Trista Ann Michaels
Eye of the Storm by Jack Higgins
Charmed (Death Escorts) by Hebert, Cambria
Agent for a Cause (The Agents for Good) by Stanton III, Guy
A Quilt for Jenna by Patrick E. Craig
Dancing on the Edge by Han Nolan